Arun Venkatesan, M.D., Ph.D.
- Associate Director, Neurology Residency Program
- Associate Professor of Neurology

https://www.hopkinsmedicine.org/profiles/results/directory/profile/0018497/arun-venkatesan
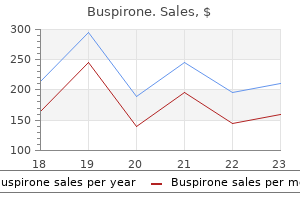
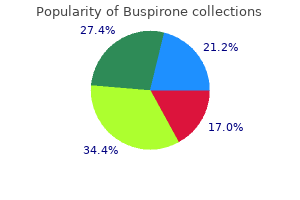
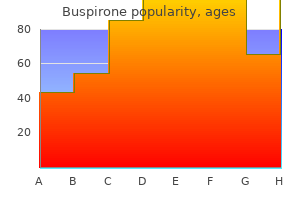
Buspirone dosages: 10 mg, 5 mg
Buspirone packs: 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Discount buspirone 5 mg free shipping
Foremost, how much "gap" may be tolerated during the therapeutic course of since sutures loosen under the influence of postoperative cyclic loads For example, after an arthroscopic rotator cuff restore, can the local tissues tolerate a small gap between tendon and bone and nonetheless obtain profitable healing of the cuff Is the critical gap affected by affected person age, systemic illness, or native degeneration (eg, tendinosis) Should the same threshold apply to suture loops which are tied for tissue-to-tissue repair similar to capsular plication to treat multidirectional shoulder instability or side-to-side repair of enormous rotator cuff ruptures However, contemplate the crucial threshold to be lower than 3 mm of hole formation to facilitate optimum tissue healing, at least for rotator cuff restore. Tendon-to-bone healing and delicate tissue-to-soft tissue healing often take someplace between 6 and 12 weeks to obtain an honest modicum of strength at the restore website (under regular physiologic conditions). Postoperative gap formation can interfere with healing on the tissue-bone interface. The subsequent logical question pertains to the in vivo masses skilled by arthroscopic repair constructs after surgical procedure. This is a very troublesome question to answer since there are little to no biomechanical data from direct postoperative measurement. Loads at the tendon-bone interface after rotator cuff repair are larger with muscle activation in comparison with passive movement. Local tissue loads could be extremely high during a sudden accidental occasion, similar to a fall, which can trigger catastrophic failure of the repair assemble. Additional sutures ought to decrease the load per suture assuming uniform load sharing for all sutures. However, this condition might be not met in vivo, where this may be very tough to achieve a superbly balanced restore. It appears logical that the "tightest" suture loop would see the greatest preliminary load, with load transferred to the subsequent tightest loop upon loosening or failure of the first loop. Peak suture-tissue forces are decreased by use of multiple sutures that distribute load evenly to multiple points of tissue fixation. In addition to requiring elevated surgical time, those may include local tissue devascularization (which may intervene with healing), extreme bulk (ie, within the joint or in the subacromial space), and tangling of sutures to be tied in relatively tight spaces. Loads within the neighborhood of 300 N would be unusual beneath most postoperative situations. However, failure of an arthroscopic knot (defined as larger than or equal to three mm of loop expansion) can happen at a lot lower masses, underneath the influence of repetitive cyclic masses. Some surgeons favor a larger distal gap within the pusher, which permits for deliberate passage over the knot. Double-holed knot pushers and self-tensioning suture gadgets are also out there, but these have largely fallen out of favor. Some knot pushers are open-sided, which allows for engagement of the suture limbs within the joint or inside the cannula. These knot pushers are inclined to disengage from the suture limb (which is normally a nuisance), and they can often rating or fret the suture (which weakens it). Some surgeons prefer to use a "sixth-finger" design, which permits for persistent tension on the knot whereas half-hitches are delivered, utilizing one instrument to accomplish both tasks. Some surgeons are snug flipping posts on sequential throws without changing the knot pusher, just by preferential pull on one suture strand or the opposite. Some surgeons prefer to bodily swap the knot pusher from one limb to the opposite, which provides a bit of time to the process. This strategy facilitates choice of the best technique by each particular person surgeon. In general, arthroscopic knots should at all times be delivered down an arthroscopic cannula. Violation of this precept can lead to substantial frustration and typically technical failure as a outcome of sutures can encircle nontarget tissues during knot supply.
Order 10 mg buspirone otc
The steps for a SutureBridge restore are essentially the identical, with the exception that more suture passes are carried out medially and all sutures are tied before linking the sutures to the lateral row. Prepare the Soft Tissues and Bone Bed Following a diagnostic arthroscopy and completion of intra-articular and/or subscapularis work, the gentle tissues and higher tuberosity bone mattress are ready. A bursectomy is accomplished and permits the surgeon to see the complete margin of the cuff tear. Any bursal leaders that connect to the internal deltoid fascia are debrided in order that the tendon edge is clearly seen. Soft tissue is removed from the larger tuberosity with an electrocautery system and a highspeed burr is used to flippantly "dust off the charcoal. Medial Anchor Placement A spinal needle identifies the correct method from the lateral acromial boarder to the medial facet of the footprint. A punch is then inserted via a percutaneous incision and used to create a bone socket for a SwiveLock C suture anchor. A SwiveLock anchor preloaded with FiberTape suture is positioned by way of the identical percutaneous portal used for punch insertion. Once the driving force tip is absolutely inserted into the prepared bone gap, the screw is delivered. The insertion sheath is backed off to verify that the highest of the anchor is seated at or just under the bone surface. Suture Passage It is important to restore the conventional length-tension relationship of the tendon. The location of medial suture placement is critical and will decide the medial-to-lateral rigidity. The authors believe that such medial placement is in massive part answerable for the stories of medial tendon failure following double-row restore. A grasper may be used to cut back the tendon in order that the surgeon can establish the perfect location for placement of the medial sutures, usually 2 to three mm lateral to the musculotendinous junction. Once the medial-tolateral location is determined, the anterior-to-posterior suture placement is evenly spaced relative to the anchor. For the SpeedBridge restore, all sutures from a medial anchor are passed via the rotator cuff first. The FiberTape sutures can simply be passed by way of the rotator cuff with an antegrade suture passer (Scorpion) and retrieved. In the SutureBridge equipment, the two ends of the FiberWire are delivered collectively in order that both FiberTape sutures limbs can be handed through the rotator cuff in a single cross. However, in most cases, the authors prefer to additionally move the eyelet safety sutures via the identical location so that a medial double-pulley restore may also be carried out. This step is accomplished with a FiberLink suture, which is used to shuttle the FiberTape and the FiberWire eyelet sutures through the rotator cuff. The free nonlooped end of the FiberLink suture is loaded onto a Scorpion, inserted by way of a lateral working portal, and passed via the rotator cuff as beforehand described. The free finish of the FiberLink is retrieved out of an anterior portal or the percutaneous portal used for anchor placement, whereas the looped finish is held outside of the lateral portal. The FiberTape and FiberWire sutures from the anteromedial anchor are then retrieved out of the lateral portal and threaded through the looped end of the FiberLink. Finally, by pulling the free finish the FiberLink, these sutures are shuttled by way of the rotator cuff at a single web site. Alternating rigidity on the sutures limbs is used to confirm that slack is eliminated and that all of the suture has been shuttled by way of the rotator cuff. Prior to acquiring lateral fixation, medial mattress stitches are tied with a double-pulley method using the #2 FiberWire security eyelet sutures from the SwiveLock anchors. This medial mattress sew supplies a medial seal between the glenohumeral joint and the rotator cuff and provides unbiased medial row fixation. The knot is delivered into the subacromial house and seated onto the rotator cuff by pulling on the other ends of the sutures. The anterior cable attachment bifurcates around the top of the bicipital groove with part of the anterior cable attachment corresponding to the anterior attachment of the supraspinatus and the other component comparable to the higher attachment of the subscapularis.
Diseases
- Woolly hair autosomal recessive
- Spastic paraparesis
- Chromosome 3, monosomy 3q27
- Rhabdomyosarcoma, embryonal
- Hyperlysinemia
- Multicentric reticulohistiocytosis
- Headache, cluster
Discount buspirone online american express
Controversial Indications Posteroinferior-dominant multidirectional instability Posterior glenohumeral instability with important glenoid or humeral bone loss Pertinent Physical Findings Posterior load and shift check: Patient is positioned supine on the analyzing desk to stabilize the scapula. The arm is positioned in roughly 20 degrees of abduction and ahead flexion. A slight axial load is first utilized to middle the humeral head in the glenoid, and the examiner then makes an attempt to translate the humeral head posteriorly. Jerk take a look at: Patient is placed supine on the analyzing desk to stabilize the scapula. The arm is then slightly adducted and a posterior axial load is utilized along the axis of the humerus. The examiner appears for a dimple or sulcus between the humeral head and acromion larger than 1 cm. If a sulcus is seen, the examiner then performs the test with the arm in external rotation to decide if the sulcus signal diminishes with rotator interval tensioning. Pertinent Imaging Three-view radiographs of shoulder: these are carefully evaluated for humeral head subluxation, reverse Hills-Sachs humeral head lesions, fractures or bony deficiency of the posterior glenoid, and glenoid retroversion. Standard arthroscopic instruments used: normal 4-mm, 30-degree arthroscope, arthroscopic shaver and burr, varied trocars and switching sticks in addition to plastic and metallic cannulas, and arthroscopic graspers and suture retrievers. It is helpful to have multiple suture passers with a selection of angles in both rightand left-facing orientations. Rotator cuff integrity is also evaluated, and glenoid rim fractures or excessive glenoid retroversion may be seen. A complete examination under anesthesia is carried out to evaluate glenohumeral instability. An inflatable bean bag is used to stabilize the affected person on this place, and the nonoperative arm is placed on an arm board. Assessment of the posterior labral and capsular structures through this anterosuperior portal is useful in identifying and precisely assessing pathology within the posteroinferior facet of the glenohumeral joint. The operative arm is then positioned in roughly forty five levels of abduction and 10 degrees of flexion and attached to the traction equipment. Ten lbs of traction is the usual, with 15 lbs reserved for larger sufferers when 10 lbs is inadequate. The arthroscope is inserted into the posterior viewing portal and commonplace glenohumeral diagnostic arthroscopy is performed. An anterior portal is created in an outside-in trend in the middle of the rotator interval. The arthroscope is then switched to the anterior portal and a switching stick is placed into the posterior portal. While viewing from the anterior portal, the anterior humeral head is thoroughly evaluated for a reverse Hill-Sachs lesion. A cannula is positioned over the posterior switching stick underneath direct arthroscopic visualization. A probe is then positioned by way of the posterior cannula, and the posterior labrum and capsule are thoroughly evaluated. It is important to notice that posterior labral harm may be much less dramatic than that generally seen with anterior Bankart lesions. After posterior capsuloligamentous pathology is confirmed, the arthroscope is then positioned back into the posterior portal. An accent anterosuperior portal is then created within the rotator interval just anterior to the main edge of supraspinatus. Viewing from the anterosuperior portal allows full visualization of the glenoid and associated capsuloligamentous constructions. The labrum could be indifferent from the posterior glenoid rim with or with out an associated bony lesion. Step 2 Access to the posteroinferior glenoid is essential for achievement during arthroscopic posterior labral repair. The standard posterior viewing portal is often too medial for posterior labral elevation, glenoid preparation, and suture anchor insertion. Furthermore, the inferior capsule may be troublesome to attain via the usual posterior portal. Therefore, an accessory inferior posterolateral working portal (posterior instability portal) is created. This portal is typically 1 to 2 cm lateral and distal to the standard posterior portal.
Cheap buspirone 10 mg online
He can also be on the Editorial/Governing Board for Arthroscopy, Knee, and Orthopedics. Ryu is a paid consultant for MedBridge, receives honoraria for lectures from Mitek, and is on the advisory board for Rotation Medical. He has editorial affiliations with Orthopedics Today and Operative Techniques in Sports Medicine. He is on the editorial or governing board for Arthroscopy and Journal of Wrist Surgery. He is an unpaid marketing consultant for Biomet, Exactech, Inc, Mitek, Rotation Medical, and Smith & Nephew. Hiroyuki Sugaya is on the speakers bureau; receives paid presentations; and is a marketing consultant, evaluator, and reviewer for DePuy Synthes and Smith & Nephew. Formation of granulation tissue For contact healing to occur a fracture should be anatomically lowered and be absolutely secure. This happens through the use of units, which cause interfragmentary compression resulting in strain environments often far less than 2%. It is formed in high strain of as a lot as one hundred pc and its formation occurs in the initial phases of secondary bone healing. Remodelling Primary bone healing occurs via the simultaneous resorption of bone by osteoclasts and manufacturing of bone by osteoblasts. This course of additionally occurs as the woven bone fashioned in secondary bone therapeutic matures to lamellar bone in the remodelling section. They form bridging osteons that mature into lamellar bone by direct remodelling Primary healing of fractures can occur either by way of contact therapeutic or by hole healing. Both processes involve an try and instantly re-establish an anatomically appropriate and biomechanically competent lamellar bone construction. Direct bone therapeutic can only happen when an anatomical restoration of the fracture fragments is achieved and rigid fixation is offered, resulting in a substantial decrease in interfragmentary strain. Bone on one aspect of the cortex must unite with bone on the opposite side of the cortex to re-establish mechanical continuity. Under these situations, cutting cones are shaped at the ends of the osteons closest to the fracture website. The tips of the cutting cones include osteoclasts that cross the fracture line, generating longitudinal cavities at a fee of 50�100 �m/day. These cavities are later filled by bone produced by osteoblasts residing at the rear of the chopping cone. This leads to the simultaneous (not sequential) generation of a bony union and the restoration of Haversian techniques formed in an axial course. The re-established Haversian methods permit for penetration of blood vessels carrying osteoblastic precursors. The bridging osteons later mature by direct remodelling into lamellar bone, leading to fracture therapeutic with out the formation of periosteal callus. In this process the fracture website is primarily stuffed by lamellar bone (akin to intramembranous ossification) oriented perpendicular to the long axis, requiring a secondary osteonal reconstruction not like the method of contact therapeutic. The major bone structure is then steadily changed by longitudinal revascularized osteons carrying osteoprogenitor cells that differentiate into osteoblasts and produce lamellar bone on every surface of the gap. This lamellar bone, nonetheless, is laid down perpendicular to the lengthy axis and is mechanically weak. This preliminary course of takes approximately 3 to eight weeks, after which a secondary remodelling resembling the contact therapeutic cascade with chopping cones takes place. Although not as intensive as endochondral remodelling, this section is necessary so as to absolutely restore the anatomical and biomechanical properties of the bone. Less than 2% Granulation tissue will form in strain environments as a lot as 100 percent; fibrous connective tissue will type up to 17%, fibrocartilage in the range 2�10%, and lamellar bone at less than 2%. Periosteal callus Periosteal callus is shaped by the identical mechanism as intramembranous ossification (the methodology through which will increase within the diameter of the bone are achieved). Periosteum has an inner loose vascular osteogenic (cambium) layer which contains pluripotent cells. Following trauma, offered that relative stability is present and the periosteum has not been extensively stripped, the pluripotent cells become osteoprogenitor cells which in turn turn into osteoblasts and bone is laid down with out first forming cartilage. It is an important a half of the preliminary haematoma and irritation phases of callus formation.
Purchase cheap buspirone on line
The roof of the third ventricle is kind ed by the body of the fornix, a pair of crura type ing a pathway that extends on all sides from the hippocampus (a a part of the tem poral lobe of the cerebral cortex) to the hypothalam us. Note: the interior capsule delineates the topographical border bet ween the diencephalon and telencephalon. The axis of the brain stem is described utilizing the sam e term s of location and course used for the longitudinal physique axis. The brainstem consist s of three brain sections, which from cranial to caudal are the m esencephalon, pons, and m edulla oblongata. Inside the cranium, the brainstem lies near the clivus, a area of the occipital bone. Visible from the out aspect in a ventral view (a) are � the cerebral peduncles (crura cerebri), composed of tracts descending to the pons, m edulla oblongata and spinal cord, � the basilar pons, containing a big tract that enters the cerebellum, � the pyram id (form ed by the pyram idal tract), and � the olive (a group of nuclei). In dorsal view (b, seen only after the cerebellum has been rem oved): � the quadrigem inal plate (tectum), with t wo paired nuclear groups for auditory and visible perform, type ing the roof plate of the m esencepahlon, � the m edulla oblongata with t wo paired tubercula type ed by the posterior funiculus nuclei, � intersection of the three paired cerebellar peduncles which border the brainstem and wager ween which lies the diam ond-shaped base of the fourth ventricle (rhom boid fossa). The rhom boid fossa is type ed partially by the pons and partially by the m edulla which is type ed by the m edulla oblongata. Note: the brainstem is the point of entry and em ergence for all true cranial nerves (for classi cation see p. C Brainstem: compartmental organization and inside construction Cross part of brainstem, superior view. The base of the brainstem usually contains giant motor tracts descending to the brainstem and the cerebellum. A continuous band of gray mat ter, the substantia nigra, is positioned directly above the cerebral peduncles. Large groups of nuclei are discovered here that serve di erent features (particularly prom inent is the pink nucleus). Multiple ascending (sensory) tracts to the telencephalon (over the thalm aus in the diencephalon) and the cerebellum and some descending tracts to the spinal additionally occupy the tegm entum. This roof area incorporates t wo superior collicular and t wo inferior collicular nuclei which play an important position in the visible and auditory pathways. Sim ilar to the telencepahlon, the cerebellar verm is and hemispheres include centrally situated white m at ter (or m edulla), surrounded by grey mat ter within the form of the cortex. The m orphological look of medulla and cortex in a midsagit tal part is identified as the abor vitae (tree of life). Em bedded inside the white m at ter are 4 paired deep cerebellar nuclei, composed of gray m at ter. The cerebellum is worried with multiple capabilities including the unconscious management of steadiness and ne motor expertise. The cerebellum is positioned dorsal to the brainstem and type s the roof of the fourth ventricle (a). Bet ween the brainstem and cerebellum on either side is a recess- cerebellopontine angle (b) which is the of clinical signi cance. Like the telencephalon, the cerebellum consists of t wo hem ispheres, which are separated by an unpaired verm is (c). The surface of hem ispheres and verm is reveals furrow-like depressions, the ssures, which separate the very thin folia from one another. Fissures and folia of the cerebellum correspond to the sulci and gyri of the telencephalon. The occulonodular lobe (b) one of many m ain subdivisions of the cerebellum, is positioned inferiorly and consists of the paired occuli, their peduncles, and the nodule of the vermis. All tract s to and from the cerebellum pass via the three paired cerebellar peduncles. The com bination of pons, cerebellum and m edulla oblongata, the buildings which surround the diam ondshaped fourth ventricle, is called the hindbrain or rhom bencephalon. The three-dim ensional illustration (b) exhibits that the time period "horn" is used to describe the threedim ensional nature of the anterior, posterior, and lateral colum ns of gray m at ter.
Syndromes
- Cryptosporidiosis
- You mail the card to a laboratory for testing.
- Excessive bleeding
- Shortness of breath
- You may only need careful observation by your doctor with repeat Pap smears every 6 to 12 months.
- Burning sensation
- Pain
- Bitter taste in the mouth
- Twitching facial muscles
- Cold packs and heat therapy may help your back pain.
Purchase buspirone 10 mg with mastercard
Location of the Hill-Sachs lesion in shoulders with recurrent anterior dislocation. Hill-Sachs "remplissage": an arthroscopic solution for the engaging Hill-Sachs lesion. Remplissage versus Latarjet for participating Hill-Sachs defects with out substantial glenoid bone loss: a biomechanical comparison. Moderate to giant engaging Hill-Sachs defects: an in vitro biomechanical comparison of the remplissage process, allograft humeral head reconstruction, and partial resurfacing arthroplasty. Chronic anterior glenohumeral instability in soccer gamers: results for a collection of 28 shoulders handled with the Latarjet procedure. Surgical therapy of anterior instability in rugby union players: scientific and radiographic results of the Latarjet-Patte process with minimum 5-year follow-up. The arthroscopic Latarjet process for the therapy of anterior shoulder instability. Neer Award 2008: Arthropathy after major anterior shoulder dislocation-223 shoulders prospectively followed up for twenty-five years. Nonoperative therapy of main anterior shoulder dislocation in patients forty years of age and youthful. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric examine. Does the presence of glenoid bone loss affect coracoid bone graft osteolysis after the Latarjet procedure A computed tomography scan research in 2 groups of patients with and without glenoid bone loss. Coracoid bone graft osteolysis after Latarjet procedure: a comparability research between two screws standard method vs mini-plate fixation. Compression of the suprascapular nerve at both the transverse scapular ligament or the spinoglenoid ligament leads to resultant posterior shoulder ache, muscle weak point, and everlasting muscle atrophy if left untreated. Early literature noted the nerve, when compressed on the transverse scapular ligament, was affected by trauma similar to a fracture by way of the scapular notch or even a proximal humerus fracture caused by a direct blow to the shoulder. It has been reported that the suprascapular nerve is the second most common isolated nerve injury seen in shoulder dislocations, second to the axillary nerve. The commonest benign lesion is a ganglion, both steady or separate from the articular labrum. The arthroscopic approach increases the ability to visualize anatomy, permits for a faster return to sports activities or actions of daily living, and is the preferred method when surgery is indicated. The morbidity and postoperative recovery following arthroscopic releases can also be less traumatic for the affected person. Compression at the spinoglenoid ligament leads to chronic conditions of atrophy of only the infraspinatus. Painless weak point in shoulder external rotation and abduction shall be detected in patients with spinoglenoid ligament compression. In patients with long-standing disease, the teres minor and serratus anterior muscle can compensate for weak spot of the infraspinatus to get hold of near-normal energy. Therefore, the cross arm adduction test may be used to assist make the diagnosis of suprascapular neuropathy at the spinoglenoid ligament. Clinical picture of a lidocaine injection to be positioned at the spinoglenoid ligament, 4 cm medial to the posterolateral nook of the acromion. Pertinent Imaging Electrodiagnostic testing with myography and nerve conduction research, while the best objective measure for a suspected analysis, are often unfavorable as this is a dynamic and never a static diagnosis. Presence or absence of supraspinatus and infraspinatus muscle atrophy and fatty infiltration could additionally be noted. Chronic denervation, seen best on T1 spin echo with increased signal intensity throughout the muscle mass, will demonstrate muscle atrophy with fatty infiltration. Suprascapular entrapment neuropathy: a clinical, anatomical and comprehensive study. Arthroscopic Suprascapular Nerve Release: the Transverse Scapular Ligament 223 Equipment 30-degree video arthroscope 18-gauge spinal needle three. To keep away from unnecessary swelling and to enhance visibility, the pump pressure is saved low at forty five mm Hg maximum. This procedure should precede any extra procedures performed on the identical shoulder that day. Step-by-Step Description: Arthroscopic Release of the Transverse Scapular Ligament Step 1 the standard subacromial portals, together with posterior, anterolateral, and lateral subacromial portals, are used for decompression at the transverse scapular ligament.
10mg buspirone overnight delivery
The taste buds are bordered by serous glands (see Bb�e) which would possibly be known also as von Ebner glands; they produce a watery secretion that retains the taste buds clear. The papillae are divided into four m orphologically distinct t ypes: b (Circum) Vallate papillae: encircled by a depression and containing plentiful style buds on their lateral surfaces c Fungiform papillae: m ushroom -shaped, located at the sides of the tongue (they exhibit m echanical receptors, therm al receptors, and style buds) d Filiform papillae: rasp-like papillae with a thick cap of keratin which are delicate to tactile stim uli e Foliate papillae: located on the posterior sides of the tongue, containing num erous style buds a hundred and eighty Head a nd Neck 5. Orga ns and Their Neurovascula r Structures Dorsum of tongue Palatoglossus St yloid course of Apex of tongue St yloglossus Mandible Hyoglossus Hyoid bone Genioglossus a Geniohyoid Lingual aponeurosis Lingual m ucosa Superior longitudinal m uscle Lingual septum Vertical m uscle of tongue Transverse m uscle of tongue C Muscles of the tong ue a Left lateral view, b anterior view of a coronal part. The extrinsic lingual m uscles embody the � � � � genioglossus, hyoglossus, palatoglossus, st yloglossus. Inferior longitudinal m uscle Hyoglossus Genioglossus the intrinsic lingual m uscles embrace the � � � � superior longitudinal m uscle, inferior longitudinal m uscle, transverse m uscle, vertical m uscle. Sublingual gland Mylohyoid b Geniohyoid the extrinsic m uscles m ove the tongue as an entire, while the intrinsic m uscles alter its shape. D Unilateral hypoglossal nerve palsy Active protrusion of the tongue with an intact hypoglossal nerve (a) and with a unilateral hypoglossal nerve lesion (b). When the hypoglossal nerve is dam aged on one side, the genioglossus m uscle is paralyzed on the a ected side. As a result, the healthy (innervated) genioglossus on the opposite facet dom inates the tongue throughout the m idline towards the a ected side. The lingual vein often runs parallel to the artery and drains into the internal jugular vein. The chorda t ympani also accommodates presynaptic, parasympathetic viscerom otor axons which synapse in the subm andibular ganglion, whose neurons in turn innervate the subm andibular and sublingual glands (see p. Apex of tongue Anterior lingual glands Frenulum Deep lingual artery and vein Lingual nerve Subm andibular duct Sublingual fold Sublingual papilla b 182 Head a nd Neck 5. Thus, a disturbance of taste sensation involving the anterior t wo-thirds of the tongue indicates the presence of a facial nerve lesion, whereas a disturbance of tactile, ache, or therm al sensation indicates a trigem inal nerve lesion (see additionally pp. The lymphatic drainage of the tongue and oral oor is m ediated by sub m ental and subm andibular teams of lymph nodes that ultim ately drain into the lymph nodes alongside the internal jugular vein (a, jugular lymph nodes). Because the lym ph nodes obtain drainage from each the ipsilateral and contralateral sides (b), tum or cells m ay becom e extensively dissem inated on this region (for instance, m etastatic squam ous cell carcinom a, particularly on the lateral border of the tongue, regularly m etastasizes to the opposite side). This sheet consists of four m uscles, all of that are situated above the hyoid bone and are thus collectively generally identified as the suprahyoid m uscles: 1. Digastric: the anterior stomach of the digastric is positioned within the oral oor region; its posterior stomach arises from the m astoid process. The tonsils are "im m unological sentinels" surrounding the passageways from the m outh and nasal cavit y to the pharynx. The lym ph follicles are distributed over all of the epithelium, showing m arked regional variations. Severe enlargement of the palatine tonsil (due to viral or bacterial an infection, as in tonsillitis) m ay signi cantly slender the outlet of the oral cavit y, inflicting di cult y in swallowing (dysphagia). It is particularly well developed in (sm all) youngsters and begins to regress at 6 or 7 years of age. Since the m outh is then const antly open during respiration at relaxation, an skilled exam iner can shortly diagnose the adenoidal condition by visual inspection. The epithelium acquires a looser texture, with plentiful lymphocytes and m acrophages. Besides the well-de ned tonsils, sm aller col-lections of lymph follicles m ay be found within the lateral bands (sal- pingopharyngeal folds). They lengthen alm ost vertically from the lateral wall to the posterior wall of the oropharynx and nasopharynx. The m ucosal surface of the pharyngeal tonsil is raised into ridges that tremendously improve it s floor space. The floor space of the palatine tonsil is elevated by deep depressions (crypt s) in the m ucosal floor (creating an lively floor area as giant as 300 cm 2). The pharyngeal m usculature consist s of the pharyngeal constrictors (details in b) and the comparatively weak pharyngeal elevators. Orga ns and Their Neurovascula r Structures Pharyngobasilar fascia Accessory m uscle bundle Superior pharyngeal constrictor Digastric m uscle, posterior stomach St ylohyoid St ylopharyngeus Hyoid bone, larger horn Middle pharyngeal constrictor Masseter m uscle, deep half Masseter m uscle, superficial part Medial pterygoid Pharyngeal raphe Inferior pharyngeal constrictor B Pharyng eal muscle tissue, posterior view As this dissection exhibits, the three pharyngeal constrictors are arranged in overlapping layers. They m eet posteriorly in the m idline alongside a vertical band of connective tissue, the pharyngeal raphe. The pharyngeal m uscles originate from the bottom of the cranium with a dense connective tissue m em brane, the pharyngobasilar fascia.
Cheap buspirone 5 mg on-line
Modified Judet strategy and minifragment fixation of scapular physique and glenoid neck fractures. The degree of harm to the acromioclavicular and the coracoclavicular ligaments as properly as the deltoid and trapezius attachments are additionally considered. The commonest classification is the Rockwood modification of the Allman and Tossy classification. They discovered that the take a look at was extra sensitive than plain radiographs at predicting important osseous lesions in these with anterior shoulder instability (sensitivity of 100 percent, specificity of 86%, constructive predictive worth of 73%, and unfavorable predictive value of 100 percent for the check versus a sensitivity of 50%, specificity of 100%, optimistic predictive worth of one hundred pc, and adverse predictive worth of 84% for plain radiographs). The bony apprehension take a look at for instability of the shoulder: a potential pilot evaluation. When judging rotational alignment of the radius on an anteroposterior radiograph the radial tuberosity should lie by which orientation in relation to the radial styloid When judging rotational alignment of the ulna on a lateral radiograph, which of the next is the right orientation of the ulnar styloid In a Galeazzi fracture, at a most of what distance from the lunate fossa of the distal radius does the radius tends to fracture Which construction is the chief stabilizer against longitudinal radioulnar migration after resection or multifragmentary fracture of the radial head A 38-year-old car mechanic has sustained an open fracture of the shaft of the fifth metacarpal of his dominant hand. He has an angulation of 50� on a lateral view but you resolve to handle it non-operatively. Which of the following statements best describes the rationale behind this strategy Malunion might be compensated by the comparatively mobile fifth carpometacarpal joint B. Which of the following is a sign for elimination of the nail for nail bed injuries Facing the ulna the radial tuberosity should face the ulna on the anteroposterior projection of the forearm. While not exclusive it tends to be true that fractures more proximal than the distal 7. The stabilizing effect of soft-tissue constraints in artificial Galeazzi fractures. Central band of the interosseous ligament the intraosseous membrane controls motion between the radius and the ulna. Median nerve dysfunction All these issues can occur, however median nerve dysfunction is extraordinarily widespread. Immobilization in a easy forearm cast Stable undisplaced fractures are appropriate for non-operative treatment. The scapholunate is often widened on radiographs as the scapholunate ligament is torn because the bones separate. Failure to debride adequately the risk of infection following open fractures with easy wounds is 1. Several of the components talked about are related to an elevated threat of infection but crucial factor is the failure to debride adequately. Middle Because the center finger is the longest it has the highest incidence of nail tip accidents. Haematoma of 50% of the nail mattress the indication for elimination of a nail for nail bed injuries is a damaged nail with disrupted edges or a haematoma affecting over 50% of the nail bed. Disruption of the iliopectineal line on an anteroposterior radiograph suggests a fracture of which of the next structures of the acetabulum Which of the following could be the preferred approach for a posterior column acetabular fracture A 45-year-old girl affected by schizophrenia jumps from a motorway bridge approximately 20 m excessive. Open reduction and inner fixation of the accidents on the following obtainable list C.
Discount 5 mg buspirone visa
In the trigem inal nerve it self, the opposite sensory bers run parallel to the pain bers but term inate in varied trigem inal nuclei (see p. Functiona l Systems Prefrontal cortex Thalam us Hypothalam us Amygdala Central grey (periaqueductal gray) m at ter Mesencephalon Anterior pretectal nucleus Locus coeruleus Raphe nuclei Descending noradrenergic and serotoninergic fibers B Pathw ays of the central descending analgesic system (after Lorke) Besides the ascending pathways that carry pain sensation to the first somatosensory cortex, there are also descending pathways that have the abilit y to suppress pain impulses. The central relay station for the descending analgesic (pain-relieving) system is the central grey (periaqueductal gray) m at ter of the mesencephalon. It is activated by a erent input from the hypothalam us, the prefrontal cortex, and the amygdaloid our bodies (part of the lim bic system, not shown). The axons from the excitatory glutam inergic neurons (red) of the central gray mat ter time period inate on serotoninergic neurons in the raphe nuclei and on noradrenergic neurons within the locus ceruleus (both proven in blue). They term inate instantly or not directly (via inhibitory neurons) on the analgesic projection neurons (second a erent neuron of the pain pathway), thereby inhibiting the additional conduction of pain impulses. Posterolateral funiculus Processing and conduction of nociceptive signals within the spinal cord Nociceptive sign conduction within the peripheral nerve Processing of nociceptive indicators within the brain Pain perception General anesthesia, psychotherapeutic techniques System ic or epidural opiates, stim ulation remedy, neurosurgery Peripheral or epidural nerven block Inflam m ation, edem a, kind ation of pain m ediators Tissue damage Im m obilization, cooling, analgesic m edication, anti-inflam m atory m edication C Pain notion and therapeutic interventions Peripheral ache m ay be brought on by native tissue injury from a bee sting, for exam ple. The inform ation on this harm is transm it ted by a quantity of relay stations to the prim ary som atosensory cortex, where the alerts are perceived as ache (translated from easy encoded impulses). The cerebellar hem ispheres and basal ganglia work in parallel to program the m ovem ent and inform the prem otor cortex of the outcomes of this planning. The prem otor cortex passes the inform ation to the prim ary m otor cortex (M1), which relays the inform ation via the pyramidal tract to the alpha m otor neuron (pyramidal motor system). The alpha m otor neuron then transm it s the inform ation to the skeletal m uscle, which rework s the program right into a specic voluntary m ovem ent. Sensorim otor capabilities provide essential suggestions during this process (How far has the m ovem ent progressed Although som e of the later gures painting the prim ary m otor cortex as the begin line for a voluntary m ovem ent, this diagram reveals that m any m otor centers are involved within the execution of a voluntary m ovem ent (including the extrapyramidal motor system, see C and D; cerebellum). For practical reasons, nonetheless, the discussion com m solely begins at the prim ary m otor cortex (M1). Association cortex Planning Cerebellar hem ispheres Basal ganglia Premotor cortex Programming M1 Execution Cerebellar interm ediary Pyram idal tract Feedback B Cortical areas with motor function: initiating a motion Lateral view of the left hemisphere. The initiation of a voluntary motion (reaching for a co ee cup) outcomes from the interaction of assorted cortical areas. The primary motor cortex (M1, Brodmann area 4) is positioned in the precentral gyrus (execution of a movement). The rostrally adjacent area 6 consists of the lateral premotor cortex and medial supplementary motor cortex (initiation of a movement). These areas provide the cortical illustration of house, which is essential in precision grasping actions and eye movements. Som atosensory inform ation Control Supplem entary m otor cortex Precentral gyrus (prim ary m otor cortex, M1) Prem otor cortex Prefrontal cortex Central sulcus Postcentral gyrus (prim ary som atosensory cortex) Posterior parietal cortex 444 Neuroa na tomy 20. Functiona l Systems Efferent fibers Motor thalam us Brainstem Pontine nuclei Corpus striatum Cortex Pallidum Basal ganglia Nuclei Cerebellum Tegm entum Red nucleus C Connections of the cortex with the basal ganglia and cerebellum: prog ramming of advanced movements the pyram idal m otor system (the prim ary m otor cortex and the pyram idal tract arising from it) is assisted by the basal ganglia and cerebellum in the planning and program m ing of com plex m ovem ents. While a erent bers of the m otor nuclei (green) project on to the basal ganglia (left) with out synapsing, the cerebellum is not directly controlled through pontine nuclei (right; see C, p. The e erent bers of the basal nuclei and cerebellum are distributed to lower structures together with the spinal wire. The significance of the basal ganglia and cerebellum in voluntary m ovem ents could be appreciated by noting the e ects of lesions in these structures. While diseases of the basal ganglia impair the initiation and execution of m ovem ent s. Spinal wire Cerebral cortex Thalamus Basal ganglia Cerebellum Brainstem Spinal cord Motor inform ation Skeletal m otor function D Simpli ed block diagram of the sensorimotor system in the management of movement Voluntary m ovem ent s require fixed feedback from the periphery (m uscle spindles, tendon organs) so as to rem ain throughout the desired lim it s. The spinal cord, brainstem, cerebellum, and cerebral cortex are the three management levels of the sensorim otor system. All inform ation from periphery, cerebellum, and the basal ganglia passes through the thalam us on its method to the cerebral cortex. The medical importance of the sensory system in m ovem ent is illustrated by the sensory ataxia that m ay happen when sensory perform is lost (see D, p.
Generic buspirone 5 mg fast delivery
They then distribute e erent bers to nuclei that control the m otor system s im portant for balance. These nuclei are positioned within the � Spinal twine (m otor support), � Cerebellum (ne management of m otor function), and � Brainstem (oculom otor nuclei for oculom otor function). E erent s from the vestibular nuclei are also distributed to the next areas: Eye Labyrinth Proprioception Vestibular nuclei Spinal cord Cerebellum � Thalam us and cortex (spatial sense) � Hypothalam us (autonom ic regulation: vom iting in response to vertigo) Note: Acute failure of the vestibular system is m anifested by rotary vertigo. Nucleus of trochlear nerve Nucleus of abducens nerve Inferior cerebellar peduncle Superior vestibular nucleus Lateral vestibular nucleus Inferior vestibular nucleus Medial vestibular nucleus Medial longitudinal fasciculus Nucleus of oculom otor nerve Medial longitudinal fasciculus Cerebellum Vestibulocerebellar fibers Lateral vestibulospinal tract C Vestibular nuclei: topographic organization and central connections Four nuclei are distinguished: � � � � Superior vestibular nucleus (of Bechterew) Lateral vestibular nucleus (of Deiters) Medial vestibular nucleus (of Schwalbe) Inferior vestibular nucleus (of Roller) � the a erent bers from the ampullary crests of the sem icircular canals term inate within the superior vestibular nucleus, the higher a half of the inferior vestibular nucleus, and the lateral vestibular nucleus. The e erent bers from the lateral vestibular nucleus move to the lateral vestibulospinal tract. This tract extends to the sacral part of the spinal twine, its axons time period inating on m otor neurons. The vestibulocerebellar bers from the opposite three nuclei act through the cerebellum to modulate m uscular tone. All 4 vestibular nuclei distribute ipsilateral and contralateral axons by way of the m edial longitudinal fasciculus to the three m otor nuclei of the nerves to the extraocular m uscles. The vestibular system has a topographic group: � the a erent bers of the saccular m acula term inate within the inferior vestibular nucleus and lateral vestibular nucleus. When these epithelial cells are chem ically stim ulated, the base of the cells releases glutam ate, which stim ulates the peripheral processes of a erent cranial nerves. Peripheral processes from pseudounipolar ganglion cells (which correspond to pseudounipolar spinal ganglion cells) time period inate on the taste buds. The central parts of those processes convey style inform ation to the gustatory a half of the nucleus of the solitary tract. Their cell bodies are situated within the geniculate ganglion for the facial nerve, in the inferior (petrosal) ganglion for the glossopharyngeal nerve, and within the inferior (nodose) ganglion for the vagus nerve. However, som e of the axons of the second neurons travel to a further interm ediate station within the brainstem, the m edial parabrachial nucleus, which in turn initiatives (as third neurons) to the thalam us, which additional projects (as fourth neurons) to the insular cortex and postcentral gyrus. Collaterals from the rst and second neurons of the gustatory a erent pathway are distributed to the superior and inferior salivatory nuclei. A erent impulses in these bers induce the secretion of saliva during eating ("salivary re ex"). Besides this purely gustatory pathway, spicy meals m ay also stim ulate trigem inal bers (not shown), which contribute to the feeling of taste. The style buds (see C) are em bedded in the epithelium of the lingual m ucosa and are positioned on the surface expansions of the lingual m ucosa- vallate papillae (printhe cipal web site, b), the fungiform papillae (c), and the foliate papillae (d). Ad- ditionally, isolated style buds are located in the m ucous m em branes of the soft palate and pharynx. The surrounding serous glands of the tongue (Ebner glands), which are m ost carefully related to the vallate papillae, constantly wash the style buds clean to enable for model spanking new tasting. Hum ans can understand ve fundamental tastes: candy, bitter, salt y, bit ter, and a fth "savory" style, referred to as um am i, which is activated by glutam ate (a style enhancer). Taste bud Gustatory pore Squam ous epthelium of the tongue C Microscopic construction of a style bud (after: Chandrashekar, Hoon et al. Processes of neurons of the three above m entioned cranial nerves, which grow into the oral m ucosa from the basal facet, induce the epithelium to di erentiate into the depicted style cells (m odi ed epithelial cells). Specialized style receptor proteins within the cell m em brane of the m icorvilli are answerable for taste notion (for particulars, see physiology textbooks). After low-m olecular-weight avored substances bind to the receptor proteins, a sign transduction is induced, which causes the release of glutam ate. This in flip excites the peripheral processes of the pseudounipolar neurons with the our bodies within the ganglia of the m entioned three cranial nerves. Based on their features, every receptor cell is specialised in one of the ve tastes (see color coding); the entire vary of the notion of taste qualities is coded inside each individual taste bud. This explains why the old notion that exact areas of the tongue are sensitive to speci c style qualities is wrong.
Real Experiences: Customer Reviews on Buspirone
Hamil, 26 years: The structures anterior to this aircraft consist of the cortex and white m at ter of the frontal lobe, each of that are easily identi ed. May start overhead throwing as maturity of therapeutic is confirmed Months 4 through 8: Return to sport if signs free, with protective power and appropriate conditioning Potential Complications Surgical problems can follow operative stabilization of the unstable shoulder. This tract extends to the sacral a half of the spinal wire, its axons term inating on m otor neurons.
Arakos, 58 years: The button (Dogbone) is attached to the 2 tapes exterior of the anterior cannula and then secured with a locking arthroscopic grasper. From the initially undi erentiated neural tube, still open on each ends (a), develop three prim ary brain vesicles (b). The modulus of elasticity is greater (stiffer) on the articular in comparability with the bursal surface and should account, partly, for the larger incidence of articular in contrast with bursal floor tears.
Mortis, 24 years: Arthroscopic view of the identical needle heading towards the transverse scapular ligament to aid in visualization of an correct landmark. Course of the axons of the higher m otor neurons: On their descending means from the telencephalon, to the decussation of the pyram ids the corticospinal bers journey by way of the � Prim ary m otor cortex posterior lim b of the interior cap sule, cerebral peduncles of the m idbrain base of the pons (basal pons) m edullary pyram id Extra pyra mida l bers in the spina l cord De nition and performance: Major motor pathways (mainly for ne motion control). I would due to this fact debride and extend the skin wound to allow supply of the fracture ends followed by meticulous debridement of any unviable tissue.
Tamkosch, 47 years: The nerve is com prised of fascicles (nerve ber bundles) which are lined by their very own connective tissue sheath- the perineurium. There are other sim ilarities relating to the further course of the spinothalam ic tracts. The healthy t ympanic m em brane has a pearly grey colour and an oval form with an average floor area of approxim ately seventy five m m 2.
Rhobar, 31 years: At 6 to 8 weeks, aggressive rehabilitation is started with a return to regular activities, normally by 12 to sixteen weeks following restore. Treatment outcomes of single- versus double-row restore for bigger than medium-sized rotator cuff tears: the effect of preoperative remnant tendon length. Newer methods are being utilized that involve supplemental scaffolds to enhance the rotator cuff restore constructs by changing or reinforcing the damaged cuff tendon.
9 of 10 - Review by Q. Kippler
Votes: 196 votes
Total customer reviews: 196
References
- Guo S, Ni N: Topical treatment for capillary hemangioma of the eyelid using beta-blocker solution, Arch Ophthalmol 128(2):255-256, 2010.
- Giraldo EA, Yaqi MA, Vaidean GD. A case-control study of stroke risk factors and outcomes in African American stroke patients with and without crack-cocaine abuse. Neurocrit Care 2012; 16:273.
- Singal AK, Jain V, Dubey M, et al: Undescended testis and torsion: is the risk understated?, Arch Dis Child 98(1):77n79, 2013.
- Shah KB, Rao K, Sawyer R, et al. The adequacy of laboratory monitoring in patients treated with spironolactone for congestive heart failure. J Am Coll Cardiol 2005;46:845.
- Eisenberg MS, Thommpson RH, Frank I, et al: Long-term renal function outcomes after radical cystectomy, J Urol 191(3):619n625, 2014.
- Horwitz M, Dufour C, Leblond P, et al. Embryonal tumors with multilayered rosettes in children: the SFCE experience. Childs Nerv Syst 2016; 32(2):299- 305.
- Walsh PC, Brendler CB, Chang T, et al: Preservation of sexual function in men during radical pelvic surgery, Md Med J 39:389-393, 1990.


