Angelo Cuzalina, MD, DDS
- Private Practice - Tulsa Surgical Arts
- President, American Academy of Cosmetic Surgery 2011
- Chairman, AACS Cosmetic Surgery Fellowship Program
- Adjunct Clinical Assistant Professor of Surgery, Oklahoma
- State University
- Tulsa, Oklahoma
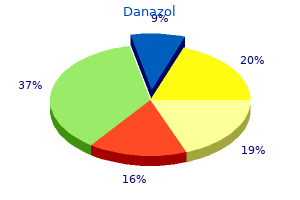
Danazol dosages: 200 mg, 100 mg, 50 mg
Danazol packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills
Purchase discount danazol
Definitive Surgery the objectives of elective definitive surgery are to clear the biliary tract of stones, to bypass or enlarge the strictures, to provide adequate biliary drainage, and the place needed, to provide percutaneous access to the biliary tract. A full and actual imaging examine to outline the location of stones and strictures and the diploma of segmental liver atrophy is obligatory in planning elective definitive therapy. For complicated circumstances, hepaticocutaneous jejunostomy, stricturoplasty, and partial hepatectomy are further procedures needed to circumvent intrahepatic ductal strictures and to eradicate impacted stones. Nonsurgical Treatment of an Acute Attack Biliary decompression could be achieved by endoscopic papillotomy (see Chapter 29) and nasobiliary catheter or large-bore endoprosthesis insertion (Lam, 1984). The drainage tubes utilized in these procedures are small, and the lumen is even smaller; these can be blocked simply in the presence of thick, infected bile and gentle stones (Takahashi et al, 1990). Because multiple strictures are sometimes present inside and out of doors the liver, a single drain is inadequate in affording whole decompression. Possible causes of ongoing sepsis embody empyema of the gallbladder with perforation and bile peritonitis, a number of undrained segmental ducts, liver abscess, and blockage of the lumen of a beforehand placed drainage tube by thick bile. By such an extension, pathology located on the confluence involving the principle proper or left duct can be readily approached. The orifice of the right posterior sectoral duct, especially when it joins the left duct, could be uncovered for removing of an impacted stone. If a stricture is discovered at this orifice, dilatation or stricturoplasty (Fan & Wong, 1996) could be performed. In this case, access to the intrahepatic ducts can be achieved by direct hepatotomy (Zhang et al, 1997). This technique causes minimal bleeding if the parenchyma is skinny however massive bleeding if the stones are deeply seated. The problem could be circumvented by electrohydraulic lithotripsy (Fan et al, 1989), which includes introduction of an electrohydraulic probe by way of the working channel of a versatile choledochoscope. Under direct visible control, the probe is introduced into contact with the stone, which is disintegrated by sparks generated by the electrohydraulic lithotripter. The lithotripter must be applied cautiously, because a probe in contact with the ductal wall might damage the wall and result in hemobilia. Cholecystectomy Emergent cholecystectomy has been recommended by some authors only when gallbladder illness is present. A high transverse incision is used, and the duodenum is recognized by its anterior relationship to the kidney. Although a supraduodenal choledochoduodenostomy suffices for a variety of the indications listed, and the anastomosis allows passage of an endoscope for analysis or remedy, the disadvantage is feasible improvement of the sump syndrome and liver abscess, as a end result of meals particles might reflux into the partially obstructed segmental duct (Rumans et al, 1987). Conversion from choledochoduodenostomy to hepaticojejunostomy could also be required in these situations. Hepaticojejunostomy is also required when a stricture is current in the widespread hepatic duct. Biliary Drainage Procedures Additional drainage procedures, corresponding to transduodenal sphincteroplasty (see Chapter 36) and choledochojejunostomy or hepaticojejunostomy (see Chapters 31 and 42), are carried out when specific indications are present. Intrahepatic strictures proximal to the hepaticojejunal anastomosis impede free drainage of bile and passage of stones. Reoperation for recurrence of stones after hepaticojejunostomy turns into more and more troublesome and dangerous. The stoma is closed and buried beneath the skin, so it may be reconstructed as a stoma for diagnostic and therapeutic purposes when recurrence of disease is suspected. A number of strategies are efficient for construction of a hepaticocutaneous jejunostomy (Hutson et al, 1984). Complete clearance of stones is sometimes unimaginable due to the presence of an enormous number of stones, or because many more stones are found solely on postoperative cholangiogram. Postoperative choledochoscopy is required via the T-tube tract, or a cutaneous stoma is required. With quite a few classes of choledochoscopy aided by electrohydraulic lithotripsy, complete stone clearance can be achieved in 90% of sufferers (Table 44. With the help of the "mother-baby" endoscope system, the whole stone removing rate is roughly 64%. Access to the biliary tract by utilizing the gastroscope through choledochoduodenostomy or interposition duodenojejunostomy has been thought-about (Cunha et al, 2002; Ramesh et al, 2003). Although these strategies have the benefit of no cutaneous stoma or percutaneous tube, both have the drawback of poor entry to the small intrahepatic ducts by the gastroscope. Hepatic Resection Partial hepatectomy is indicated for destroyed liver segments, multiple cholangitic liver abscesses, and concomitant cholangiocarcinoma (Cheung & Kwok, 2005; Co et al.

Order danazol 50 mg with mastercard
Intravenous Anesthetics and Muscle Relaxants Inhaled anesthetics supply all the elements wanted for anesthesia in a single package, but at present most anesthesiologists select a quantity of drugs to reach their targets: immobility, amnesia, suppression of autonomic reflexes, muscle leisure, and analgesia. Anesthesiologists using multiple medicine benefit from the interactions of medicine with completely different mechanisms of action however similar therapeutic results. The therapeutic aim of the anesthetic can usually be achieved with less toxicity and faster restoration than when the person medication are used alone in greater doses. The liver plays a significant function in biotransformation, the process through which medication are damaged down into metabolites that may be more simply eliminated. High-extraction drugs (ketamine, flumazenil, morphine, fentanyl, sufentanil, lidocaine) are immediately associated to liver blood circulate and basically cleared as they cross via the liver. Protein binding, enzymatic induction, intrahepatic shunting, and the effect of anesthetics on liver blood circulate might have an result on the elimination of medication with a high-extraction rate. Reductions in metabolic clearance lead to will increase of peak drug level with minimal change in the elimination half-life. However, in the modern period of bloodless hepatic resection, to avoid the morbidity related to central vein cannulation, our clinical apply has deserted the routine use of central venous traces. Patients should nonetheless be prepared for large-volume transfusion, although that is sometimes needed. Close cooperation between the anesthesiologist and the surgeon continues so that likely difficulties can be anticipated and acceptable measures could be taken. Phase 1: Prehepatic Prehepatic resection begins at anesthesia induction and ends at the completion of parenchymal transection and hemostasis. During this phase, influx control of the portal vein and hepatic artery are achieved, and the vena cava and hepatic veins are dissected. Sixty % of the time, hepatic parenchymal transection is performed with intermittent influx occlusion (Pringle technique) applied (Kingham et al, 2014). This phase avoids fluid extra and takes benefit of the vasodilatory effects of anesthetic medicine. Preoperative overnight fluid alternative is withheld, and upkeep fluid requirement at 1 mL/kg/hr of balanced crystalloid answer is infused till the liver resection is completed. Intermittently, small fluid boluses or vasoactive drugs could also be given to preserve hemodynamic stability. Some extent of permissive oliguria as a outcome of decreases in antidiuretic hormone or permissive relative hypotension while peripheral tone is decreased will allow for continued minimal fluid infusion until the specimen is delivered. Isoflurane offers vasodilation with minimal myocardial despair (Schwinn et al, 1990). Consistent with its minimal impact on cardiac output and systemic stress, fentanyl has no effect on liver blood move and oxygen supply and, given its lack of toxic metabolites, could be administered just like any abdominal surgery without any dosing discount (Trescot et al, 2008). The blood loss ensuing from a vascular damage is immediately proportional to the stress gradient across the vessel wall and the fourth power of the radius of the injury. Twenty years ago, the authors developed and reported a easy, efficient, and reproducible method for reducing the intraoperative blood loss in patients present process liver resection based mostly on fluid restriction and the vasodilatory results of anesthestic brokers (Melendez et al, 1998). These patients typically required intraoperative dopamine for systemic stress assist. The method seemed cumbersome; adding an pointless stage of complexity to an already challenging scenario. Despite this, both approaches contributed to improved outcomes and continue to be practiced at main institutions (Correa-Gallego et al, 2015; Dunki-Jacobs et al, 2013; Jones et al, 2013; Lin et al, 2014). Postresection: Phase 2 Posthepatic resection, the second section, begins as quickly as the specimen has been delivered and hemostasis secured. During this part, the goal of fluid prescription is to go away the operating room with a normovolemic affected person. Liver surgical procedure exposes sufferers to periods of cardiovascular insufficiency, either due to anesthesia-induced lack of vasomotor tone and baroreceptor responsiveness or because of blood loss and mechanical obstruction to blood circulate. In all cases, stroke quantity will fall in addition to international oxygen delivery to the tissues. Because surgery also creates a cytokine storm, the mixture of relative hypoperfusion and immune modulation will alter the microcirculation, causing subclinical damage. The optimal perioperative fluid resuscitation technique for liver resections stays undefined. Splanchnic veins, with their larger density of -adrenergic receptors, play the main position in maintaining a ratio between confused (Vs) and unstressed blood quantity (Vu) (Gelman, 2008). Vu is hemodynamically inactive, however when venoconstriction modifications it, that is equal to a transfusion of a significant quantity of blood.
Cheap danazol 200 mg with amex
Tabrizian P, et al: Hepatic resection for major hepatolithiasis: a single-center Western experience, J Am Coll Surg 215:622�626, 2012. Takada T, et al: Classification and remedy of intrahepatic calcali, Jap J Gastroenterol Surg 11:769�774, 1978. Takada T, et al: Technique and management of percutaneous transhepatic cholangial drainage for treating an obstructive jaundice, Hepatogastroenterology forty two:317�322, 1995. Takeshita N, et al: Forty-year expertise with flow-diversion surgery for patients with congenital choledochal cysts with pancreaticobiliary maljunction at a single institution, Ann Surg 254:1050�1053, 2011. Tanaka M, et al: Divergent effects of endoscopic sphincterotomy on the long-term outcome of hepatolithiasis, Gastrointest Endosc forty three:33� 37, 1996. Tanaka K, et al: Portal vein obstruction accompanied by intrahepatic stones, Angiology forty seven:1151�1156, 1996. Tashiro S, et al; Committee for Registration of the Japanese Study Group on Pancreaticobiliary Malfunction: Pancreaticobiliary malfunction: retrospective and nationwide survey in Japan, J Hepatobiliary Pancreat Surg 10:345�351, 2003. Tocchi A, et al: Late growth of bile duct cancer in sufferers who had biliary-enteric drainage for benign disease: a follow-up examine of greater than 1,000 patients, Ann Surg 234:210�214, 2001. Trauner M, et al: Molecular pathogenesis of cholestasis, N Engl J Med 339:1217�1227, 1998. Tsuchida Y, et al: Development of intrahepatic biliary stones after excision of choledochal cysts, J Pediatr Surg 37:165�167, 2002. Tsunoda T, et al: Long-term results of surgical therapy for intrahepatic stones, Jpn J Surg 15:455�462, 1985. Tsuyuguchi T, et al: Ten-year long-term outcomes after non-surgical administration of hepatolithiasis, including instances with choledochoenterostomy, J Hepatobiliary Pancreat Sci 21:795�800, 2014. Uchiyama K, et al: Indication and process for remedy of hepatolithiasis, Arch Surg 137:149�153, 2002. Uchiyama K, et al: Reducing residual and recurrent stones by hepatectomy for hepatolithiasis, J Gastrointest Surg 11:626�630, 2007. Uenishi T, et al: Outcomes of hepatic resection for hepatolithiasis, Am J Surg 198:199�202, 2009. Uno K, et al: Development of intrahepatic cholelithiasis lengthy after main excision of choledochal cysts, J Am Coll Surg 183:583�588, 1996. Vetrone G, et al: Surgical remedy for hepatolithiasis: a Western expertise, J Am Coll Surg 202:306�312, 2006. Watanabe Y, et al: Bile duct most cancers developed after cyst excision for choledochal cyst, J Hepatobiliary Pancreat Surg 6:207�212, 1999. Yamakawa T, et al: Intrahepatic stones and postoperative choledochoscopy, Gastroenterol Jpn 15:577�583, 1980. Yamashita N, et al: Composition of intrahepatic calculi-etiological significance, Dig Dis Sci 33:449�453, 1988. Yang T, et al: Hepatectomy for bilateral major hepatolithiasis: a cohort research, Ann Surg 251:84�90, 2010. Yarmuch J, et al: Result of surgical treatment in patients with Western intrahepatic lithiasis, Hepatogastroenterology 36:128�131, 1989. Zen Y, et al: Different expression patterns of mucin core proteins and cytokeratins during intrahepatic cholangiocarcinogenesis from biliary intraepithelial neoplasia and intraductal papillary neoplasm of the bile duct: an immunohistochemical examine of a hundred and ten cases of hepatolithiasis, J Hepatol 44:350�358, 2006. Zhou F, et al: Laparoscopic hepatectomy is associated with the next incident frequency in hepatolithiasis patients, Surg Today 43:1371� 1381, 2013. The illness could contain all or any parts of the extrahepatic biliary system and causes a progressive obstruction of the biliary tree, resulting in cholestasis, cirrhosis, and, in the end, death within the first several years of life if left untreated. To date, nevertheless, no identified mutation has been proven to cause biliary atresia in animal fashions, thereby underscoring the importance of the interplay between genes and surroundings. Although the production and results of these cytokines are predominantly within affected tissues, serum levels of these and other inflammatory markers have been studied to identify possible biomarkers of illness severity. This hypothesis has been supported by work that has identified polymorphisms in genes that regulate the metabolism of inflammatory cytokines as well as contribute to the event of biliary fibrosis (Garcia-Barcelo et al, 2010).
Order generic danazol pills
Felekouras E, et al: Malignant carcinoid tumor of the cystic duct: a rare explanation for bile duct obstruction, Hepatobiliary Pancreat Dis Int eight:640�646, 2009. Ghazale A, et al: Immunoglobulin G4-associated cholangitis: clinical profile and response to remedy, Gastroenterology 134:706�715, 2008. Hao L, et al: Carcinoid tumor of the common bile duct producing gastrin and serotonin, J Clin Gastroenterol 23:63�65, 1996. Hermina M, et al: Carcinoid tumor of the cystic duct, Pathol Res Pract 195:707�709, discussion 710, 1999. Kalaitzakis E, Sturgess R: Biliary leiomyoma recognized by Spyglass cholangioscopy (with video), Gastrointest Endosc 74:409�410, 2011. Karakozis S, et al: Granular cell tumors of the biliary tree, Surgery 128:113�115, 2000. Khalid K, et al: Granular cell tumour of the ampulla of Vater, J Postgrad Med 51:36�38, 2005. Koea J, et al: Differential prognosis of stenosing lesions at the hepatic hilus, World J Surg 28:466�470, 2004. Kozuka S, et al: Evolution of carcinoma within the extrahepatic bile ducts, Cancer fifty four:65�72, 1984. Ligato S, et al: Primary carcinoid tumor of the widespread hepatic duct: a rare case with immunohistochemical and molecular findings, Oncol Rep thirteen:543�546, 2005. Loh A, et al: Solitary benign papilloma (papillary adenoma) of the cystic duct: a uncommon cause of biliary colic, Br J Clin Pract 48:167�168, 1994. Mandujano-Vera G, et al: Gastrinoma of the common bile duct: immunohistochemical and ultrastructural examine of a case, J Clin Gastroenterol 20:321�324, 1995. Miyano T, et al: Adenoma and stone formation of the biliary tract in puppies that had choledochopancreatic anastomosis, J Pediatr Surg 24:539�542, 1989. Moore S, et al: Adenosquamous carcinoma of the liver arising in biliary cystadenocarcinoma: clinical, radiologic, and pathologic options with evaluate of the literature, J Clin Gastroenterol 6:267�275, 1984. Mukai H, et al: Tumors of the papilla and distal widespread bile duct: diagnosis and staging by endoscopic ultrasonography, Gastrointest Endosc Clin N Am 5:763�772, 1995. Nesi G, et al: Well-differentiated endocrine tumor of the distal common bile duct: a case research and literature evaluation, Virchows Arch 449:104� 111, 2006. Oden B: Neurinoma of the frequent bile duct: report of a case, Acta Chir Scand 108:393�397, 1955. Ohta H, et al: Biliary papillomatosis with the purpose mutation of K-ras gene arising in congenital choledochal cyst, Gastroenterology 105: 1209�1212, 1993. Quispel R, et al: Heterotopic gastric tissue mimicking malignant biliary obstruction, Gastrointest Endosc sixty two:170�172, 2005. Terada T, Nakanuma Y: Immunohistochemical demonstration of pancreatic alpha-amylase and trypsin in intrahepatic bile ducts and peribiliary glands, Hepatology 14:1129�1135, 1991. Thomsen P, et al: Biliary cystadenoma of the frequent bile duct with secondary biliary cirrhosis: report of a case, Acta Med Scand 216: 327�330, 1984. Van Steenbergen W, et al: Cystadenoma of the frequent bile duct demonstrated by endoscopic retrograde cholangiography: an unusual reason for extrahepatic obstruction, Am J Gastroenterol 79:466� 470, 1984. Vitaux J, et al: Carcinoid tumor of the widespread bile duct, Am J Gastroenterol seventy six:360�362, 1981. Wakai T, et al: Clinicopathological features of benign biliary strictures masquerading as biliary malignancy, Am Surg 78:1388�1391, 2012. Wardell D: Small fatty growths obstructing cystic and common ducts, Lancet 94:407, 1869. Whittaker L, et al: Heterotopic gastric mucosa within the wall of the cystic duct: report of a case, Surgery 62:382�385, 1967. Yamaoka K, et al: Leiomyoma of the widespread bile duct, Am J Gastroenterol 88:469�470, 1993. Yoshida K, et al: Chronic pancreatitis attributable to an autoimmune abnormality: proposal of the concept of autoimmune pancreatitis, Dig Dis Sci forty:1561�1568, 1995. Zen Y, et al: Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas, Hepatology forty four:1333�1343, 2006. Peter Kingham Gallbladder cancer, although rare, is the most common of biliary tract malignancy (Carriaga & Henson, 1995). It historically has been thought-about an incurable disease with an especially poor prognosis. Gallbladder cancer is usually discovered by the way after cholecystectomy performed for presumed benign illness.
Order danazol 200 mg with visa
Such methodologic shortcomings make it troublesome to make recommendations based on this research. Percutaneous transhepatic cholecystostomy for acute acalculous hemorrhagic cholecystitis. Thecysticductwaspatent,andthere was unimpeded move of contrast material into the duodenum. The authors pair-matched sufferers for age, intercourse, race, body mass index, diabetes, and sepsis. It can additionally be difficult to draw a statistically sound conclusion from such a small sample dimension. Two case series describe such an approach: In 24 (Lee et al, 1991) and 82 patients (Boland et al, 1994), cholecystostomy resulted in decision of sepsis in 58% and 51% of sufferers, respectively. Drainage versus aspiration: Drainage has been demonstrated to be superior to simple aspiration of the acutely infected gallbladder in a single randomized trial (Ito et al, 2004) and is currently most generally used. Approach: Patient preparation consists of skin disinfection and normal sterile precautions, procedural sedation, and either prophylactic administration or prepared availability of atropine, as vagal reactions have been documented (Little et al, 2013). After the planned anatomic course is identified, the gallbladder is entered using a finder needle, and a guidewire is inserted into it, with a measurement 7- to 10-Fr pigtail catheter inserted over the guidewire using a Seldinger approach. Other catheters, such as a central venous catheter, can be utilized in lieu of a pigtail catheter and could additionally be of use in sure institutional settings, but data on catheter displacement and patency occasions with these different choices are limited (Park et al, 2005). A catheter placed by transhepatic entry is most well-liked to the transperitoneal route. The evidence to support this method is scarce, and no giant cohort or managed trials has examined this query. Chiappetta Porras and colleagues (2009) described a cohort of 122 (Technical Aspects and Complications) for biliary colic in the first trimester, 4 cholecystostomies in the first trimester for cholecystitis, and 4 gallbladder aspirations within the third trimester (three for biliary colic and one for cholecystitis. The transhepatic approach is safer because it avoids the peritoneum in sufferers with significant ascites or bowel interposition (Ginat & Saad, 2008). Following catheter withdrawal, 3% of patients experience severe bile peritonitis, and another 3% experience a light symptomatic biliary leak (Wise et al, 2005). In the cohort described by Smith and colleagues (2013), catheter-related complications occurred in 14. These complications had been managed mostly with tube repositioning or upsizing, and none required operation. However, its use was restricted to sufferers with lower than three ldl cholesterol stones of measurement 2 cm or less, and it required a quantity of remedies over months. Moreover, it has been confirmed to not be a cost-effective method (Barkun et al, 1997), and its use has been largely deserted. Only four patients have been described on this examine, and no data on long-term patency of this technique was described. A small collection has described the feasibility of endoscopic ultrasound-guided transduodenal drainage of the gallbladder; nonetheless, this expertise has not been reproduced to date (Lee et al, 2007). Management of the Percutaneous Cholecystectomy Catheter and the Gallbladder As already said, the catheter tract usually matures after 2 weeks for transhepatic catheters and after 3 weeks for transperitoneal drains. Gallstones and Gallbladder Chapter 34 Percutaneous therapy of gallbladder disease 568. Aky�rek N, et al: Management of acute calculous cholecystitis in highrisk sufferers: percutaneous cholecystotomy followed by early laparoscopic cholecystectomy, Surg Laparosc Endosc Percutan Tech 15(6): 315�320, 2005. Allmendinger N, et al: Percutaneous cholecystostomy treatment of acute cholecystitis in being pregnant, Obstet Gynecol 86(4 Pt 2):653�654, 1995. Cesmeli E, et al: Gallstone recurrence after profitable shock wave therapy: the magnitude of the problem and the predictive components, Am J Gastroenterol 94(2):474�479, 1999. Glenn F: Cholecystostomy in the high danger affected person with biliary tract illness, Ann Surg 185(2):185�191, 1977. Li M, et al: Percutaneous cholecystostomy is a definitive therapy for acute cholecystitis in elderly high-risk patients, Am Surg 79(5):524� 527, 2013. Loberant N, et al: Comparison of early outcome from transperitoneal versus transhepatic percutaneous cholecystostomy, Hepatogastroenterology 57(97):12�17, 2010. Simorov A, et al: Emergent cholecystostomy is superior to open cholecystectomy in extraordinarily unwell sufferers with acalculous cholecystitis: a big multicenter end result research, Am J Surg 206(6):935�940, dialogue 940-931, 2013. Zehetner J, et al: Percutaneous cholecystostomy versus laparoscopic cholecystectomy in patients with acute cholecystitis and failed conservative administration: a matched-pair evaluation, Surg Laparosc Endosc Percutan Tech 24(6):523�527, 2014.
Purchase danazol overnight delivery
However, general tips are for antibiotic therapy to proceed until biliary obstruction is totally relieved, biochemical liver operate exams have improved or normalized, and the affected person is afebrile for at least forty eight hours. Biliary Infection and Infestation Chapter forty three Cholangitis 717 Patients in danger for recurrent cholangitis, similar to these with residual calculi or incompletely relieved obstruction from any trigger, should stay on oral antibiotics until the underlying reason for cholangitis is completely treated. Acceptable oral antibiotics for most of these patients embrace trimethoprim/ sulfamethoxazole and levofloxacin or ciprofloxacin alone or together with metronidazole. The major downside is the high gear price, fragility of the probe, low depth of penetration, and operator experience. The arterial phase might reveal peripheral or periductal hypervascularization (Arai et al, 2003). Transabdominal Ultrasound Transabdominal ultrasound (see Chapter 15) is the least costly and most universally out there imaging modality to consider the biliary tree and gallbladder. Direct Cholangiography Although traditionally thought-about the reference radiologic modality, direct cholangiography (see Chapter 20) for purely diagnostic functions has been supplanted by much less invasive crosssectional imaging alternate options, which also provide further anatomic detail associated to adjacent organs to permit a more full evaluation. Retrograde or percutaneous cholangiography is essentially limited to step one of a therapeutic process (Gallix et al, 2006) (see Chapters 29, 30, and 52). In addition to its inferior image quality, there are numerous problems associated with the usage of direct cholangiography, including biliary infection, pancreatitis, and hemorrhage (Vidal et al, 2004). Contrast is then injected to opacify the biliary tree and to establish the level/site of obstruction. The biliary tree could be efficiently visualized in near 100 percent of patients with dilated ducts and in 60% to 80% of sufferers with nondilated ducts (Tse et al, 2006). It is superb at figuring out the extent and reason for biliary obstruction, in addition to distinguishing benign from malignant lesions. The general fee for main problems is lower than 5%, with a mortality rate of 0. When the obstruction is believed to be below the bile duct bifurcation, the preferred preliminary method is endoscopic (Kumar et al, 2004). These pointers helped to facilitate evidence-based care in patients with cholangitis (Takada et al, 2007). In 2013, an up to date model was printed (Takada et al, 2013), giving special attention to new diagnostic criteria and severity evaluation standards. If the patient has gentle to average cholangitis and is steady, an effort can be made to definitively clear the duct of calculi. The procedure must be carried out in a monitored setting (endoscopy laboratory, intensive care unit, or operating theater) beneath either aware sedation or general anesthesia. In acutely ill or septic patients, biliary decompression ought to be obtained with the least amount of manipulation and effort, and extended maneuvers to remove calculi or carry out sphincterotomy should be averted. A handy method of decompression is with exterior nasobiliary drainage, a drainage procedure done by putting a 5- to 7-Fr tube using a guidewire method. External nasobiliary drainage has the benefit of being an efficient drainage software, with out the need of a sphincterotomy, and it offers access for biliary cultures. A review of these strategies was revealed in 2007 with the Tokyo tips (Tsuyuguchi et al, 2007) (see Chapters 36 and 37). The most well-liked technique and route to relieve biliary obstruction, and the ultimate word success of biliary drainage, depends upon numerous elements that embrace availability of the technique (endoscopic, percutaneous, or operative), local expertise, etiology, location and severity of obstruction, and the presence of C. Two stent shapes are available: a straight kind with flaps on each side and a pigtail kind to prevent dislocation. Advantages of this approach include minimal or absent discomfort and limited electrolyte or fluid shifts relative to transnasal biliary drainage. Disadvantages embody the potential for stent clogging or loss of patency, danger of dislodgement, and the technical disadvantage for a sphincterotomy when a stent bigger than 7 Fr is inserted. Morbidity and mortality rates are a lot higher with sphincterotomy than with nasobiliary catheter drainage when patients are critically ill (Boender et al, 1995; Chawla et al, 1994; Leese et al, 1986). Most notable was the remark that the patency rates for biliary stents at 1, three, 6, and 12 months have been 97. As acknowledged, emergent sphincterotomy to decompress the bile duct should be avoided in septic sufferers, and particularly in elderly patients, because of potentially high mortality rates (18.
Cheap danazol 200 mg fast delivery
Secondary Hepatolithiasis Secondary hepatolithiasis associated with past biliary surgery and congential biliary malformation are examples where the etiology could be presumed (Kim et al, 1995). Intrahepatic stones are detected in 12% to 17% of grownup patients with congenital choledochal cysts (Matsumoto et al, 2003; Morine et al, 2013). With latest will increase in hepatobiliary surgery and increased long-term survival, secondary hepatolithiasis as a outcome of stenosis of bilioenteric or duct-to-duct biliary anastomoses has increased (Pitt et al, 1994; Schmidt et al, 2002). Special attention has targeted on congenital choledochal cysts as a condition typically associated with both intrahepatic bile duct strictures and biliary dilation. Congenital choledochal cysts are related to intrahepatic stones (Fujii et al, 1997) in addition to a excessive incidence of biliary tract carcinoma (10. Bile contamination related to biliary strictures, anastomotic strictures, and hepaticojejununal (Rouxen-Y) anastomosis may be contributing elements (Kaneko et al, 2005), however much remains unknown about the mechanisms of onset. In addition to the increased potential of carcinogenesis as a result of long-term stimulation of biliary mucosa by pancreatic juice, bilioenteric anastomosis itself might speed up carcinogenesis because of irritation by contaminated bile, even in benign conditions (Bettschart et al, 2002; Hakamada et al, 1997; Tocchi et al, 2001) (see Chapter 51). The risk of subsequent biliary malignancy in sufferers undergoing cyst excision for congenital choledochal cysts has been reported as 0. Cholangiocarcinoma the event of cholangiocarcinoma in patients with hepatolithiasis is associated with poor long-term outcomes (see Chapter 51). The incidence of cholangiocarcinoma in patients with hepatolithiasis reported from Asian centers ranges from 2. In distinction, hepatolithiasis is unusual in Western countries, with an incidence up to 2. Vetrone and colleagues (2006) found just one case with intramucosal adenocarcinoma of the extrahepatic bile duct out of twenty-two patients with hepatolithiasis who underwent surgical therapy. On the opposite hand, Tabrizian and colleagues (2012) reported a much greater incidence of concomitant cholangiocarcinoma of 23. Also, Al-Sukhni and colleagues (2008) reported that cholangiocarcinoma was recognized in 5 of forty two (12%) sufferers during a 20-year examine period. Guglielmi and colleagues (2014) prospectively collected a cohort of 161 sufferers with hepatolithiasis from five Italian tertiary hepatobiliary centers. Although the affiliation of hepatolithiasis and cholangiocarcinoma is nicely recognized, the precise mechanism of carcinogenesis is still unclear. Persistent irritation because of cholangitis causes repeated tissue injury and regeneration. Hyperplastic epithelial cells typically showed a papillomatous or adenomatous sample, which was regularly related to the presence of stones (Koga et al, 1985). Ohta and colleagues (1991) reported that varied degrees of hyperplastic biliary epithelium have been associated with chronic proliferative cholangitis and existed round impacted stones. Mucosal dysplasia with expression of mucin core proteins and cytokeratins could also be a precursor to cholangiocarcinoma (Zen Y, et al, 2006). There has been no clear symptom or medical presentation associated with the presence cholangiocarcinoma in sufferers with hepatolithiasis. Therefore the risk of coexisting cholangiocarcinoma must be considered in all circumstances, but particularly so with unusual shows, such as weight reduction, anemia, or intractable pain (Sheen-Chen, 1991). Chijiiwa and colleagues (1995) reported that, among 85 patients with hepatolithiasis, 6 (7%) died of cholangiocarcinoma during a mean follow-up interval of 6 years. Cheon et al (2009) also reported that the speed of late improvement of cholangiocarcinoma in sufferers with intrahepatic stones during follow-up was 4. The imply interval from the preliminary treatment to the development of cholangiocarcinoma was 10. Half of the patients developed cholangiocarcinomas at a website completely different from the preliminary site of hepatolithiasis. According to a Japanese survey, age older than sixty five years and stone elimination as the one preliminary remedy have been vital threat factors for the subsequent improvement of cholangiocarcinoma (Suzuki Y et al. Further subgroup analysis revealed that age older than 65 years and the presence of biliary stricture had been important risk factors for the development of cholangiocarcinoma in sufferers with a history of bilioenteric anatomosis. In hepatolithiasis patients without a history of a bilioenteric anatomosis, left lobe location and stone recurrence have been vital danger components for the event of cholangiocarcinoma.
References
- Ozisik H, Yurekli BS, Simsir IY, et al: Testicular Adrenal Rest Tumor (TART) in congenital adrenal hyperplasia, Eur J Med Genet 60:489n493, 2017.
- Kojima T, Takahashi H, Parra-Blanco A, et al. Diagnosis of submucosal tumor of the upper GI tract by endoscopic resection. Gastrointest Endosc. 1999;50:516-522.
- Cai Z, Zhong H, Bosch-Marce M, et al: Complete loss of ischaemic preconditioninginduced cardioprotection in mice with partial deficiency of HIF-1 alpha. Cardiovasc Res 2008;77:463-470.
- Lorsomradee S, Cromheecke S, De Hert SG: Uncalibrated arterial pulse contour analysis versus continuous thermodilution technique: Effects of alterations in arterial waveform, J Cardiothorac Vasc Anesth 21:636-643, 2007.
- Vinceti M, Dennert G, Crespi CM, et al: Selenium for preventing cancer, Cochrane Database Syst Rev (3):CD005195, 2014.
- Bursztyn M, Mekler J, Ben-Ishay. The siesta and blood pressure: different hemodynamics of the morning and afternoon awakening. Am J Hyperten 2005;8(4, Part 2):164A. Haimov I, Lavie P. Circadian characteristics of sleep propensity function in healthy elderly: a comparison with young adults. Sleep 1997;20(4): 294-300.


